Laminitis is a common and debilitating condition that can result in recurrent episodes of varying degrees of lameness which, in severe cases, may require euthanasia on the humane grounds of incurable pain and suffering. In recent years our rethinking of laminitis has changed and it is now considered, in most cases, to be a syndrome in association with a disease affecting the whole body, rather than a primary disease in its own right.

What is laminitis?
In its simplest form, laminitis is damage to or failure of the sensitive layers (laminae) of the hoof. Within the hoof, the coffin bone is suspended by these interdigitating laminae. When these become damaged, it causes pain, inflammation and the formation of gaps between laminae. Mild cases may be resolved without any lasting effects on the laminae but, if the inflammation is more severe and progressive, the laminae may lose their blood supply and die, resulting in the loss of support between the pedal bone and hoof wall which, in turn, leads to rotation and/or sinking of the pedal bone within the hoof. In its severest form, the tip of the pedal bone can penetrate the sole itself, necessitating euthanasia.
What causes laminitis?
The causes of laminitis fall into three broad categories:
1) Endocrinopathic – around 90% of laminitis cases have an endocrine cause, e.g. Cushing’s Syndrome (PPID or Pars Pituitary Intermedia Dysfunction) or Equine Metabolic Syndrome (EMS) / Insulin dysregulation (ID). It is now thought that pasture-associated laminitis is an endocrine disorder in which affected animals have an abnormal insulin response to the sugars in grass.
2) SIRS (Systemic Inflammatory Response Syndrome) – this is where laminitis is secondary to a primary septic/inflammatory illness such as colitis, peritonitis, retained placenta or carbohydrate overload. Horses with SIRS will be systemically unwell.
3) Supporting limb laminitis – severe, long-standing, non-weightbearing lameness (e.g. a fracture), can cause laminitis in the opposite leg as a result of excessive loading of that limb.
Other potential causes of laminitis include neglected feet/poor trimming resulting in long toe/low heel conformation and excessive concussion due to fast exercise on hard ground
What are the signs?
In the mildest cases, horses may present with nothing more than a slightly pottery gait. The forelimbs are most commonly affected but there are cases where only the hindlimbs are affected or where all limbs are affected. Often one foot appears more severely affected than the others. Affected feet are usually warmer and have an increased digital pulse. If you are not sure how to feel for a digital pulse, it is worth learning how to do so; your Vet will be able to show you this. More severe signs of laminitis include:
- Laminitic stance – where the horse stands with his hindlimbs well under his body and leans back in an attempt to take the weight off his front feet
- Refusal to pick up feet
- Landing heel first when walking
- Reluctance to move
- Lying down more frequently
Horses that have suffered from laminitis are more prone to further episodes. Those that have recovered from laminitis often have permanent changes to their feet; the heels become long and the soles become convex rather than concave. They also develop divergent hoof rings (which are wider at the heels than the toes) due to abnormal hoof growth and are more prone to hoof wall cracks.
Emergency treatment for laminitis
I cannot stress how important it is to call your Vet as soon as you suspect laminitis. Early intervention and prompt treatment can hugely affect the course of the condition and potentially save your horse’s life. Your Vet will advise you on the best course of treatment but this will usually include some or all of the following:
- Removing the horse from grass and resting him in a stable
- Providing a deep, supportive bedding, e.g. shavings
- Supporting the feet if the bedding is not providing enough support (e.g. with styrofoam pads, hoof boots)
- Administering pain relief/anti-inflammatories, e.g. phenylbutazone
- Applying cold therapy to the feet to reduce inflammation and pain
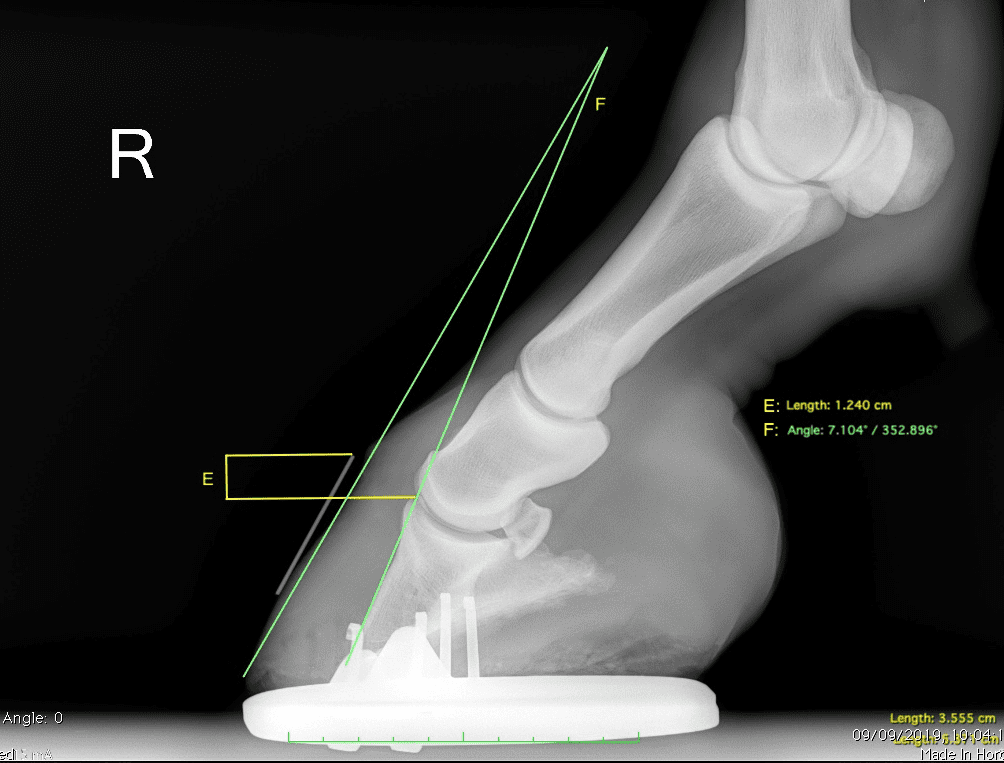
I strongly advise that, with the exception of the very mildest of cases, any horse suffering from laminitis should have foot x-rays taken to assess the degree of rotation/sinking of the pedal bone. Quite often, the severity of the symptoms shown by the horse can be hugely different from the changes seen on x-ray; donkeys are notorious for only showing mild signs of pain despite having horrendous changes on x-ray. X-rays will give your farrier a guide as to how best to trim and/or shoe your horse to make him more comfortable and can also assist your Vet in making a more accurate prognosis as to your horse’s recovery.
For the vast majority of cases, I would also advise that blood tests are performed for both PPID and EMS as, if these are implicated in the cause of laminitis, treatment of the laminitis will not be successful without the treatment of the underlying condition. The same principle applies to SIRS-related laminitis or supporting limb laminitis; treating the laminitis itself is merely the tip of the iceberg.
Prevention of laminitis
Prevent laminitis by ensuring your horse:
1) Is not overweight – if necessary, restrict grazing by using a muzzle, strip grazing or setting up a track grazing system and only allow access to grazing when sugar levels are likely to be lowest. Many Vets and feed manufacturers will happily visit your yard with a mobile weighbridge and assess your horse’s weight and body condition score and advise you on suitable feeding/management
2) Is regularly exercised (providing he is sound enough to do so)
3) Is monitored for signs of PPID or EMS (your Vet will be able to discuss with you if your horse is at risk of these)
Laminitis is an extremely painful and potentially life-threatening condition and I cannot emphasise enough how important prevention and early intervention are in achieving a successful outcome. If you suspect your horse may have laminitis, contact your Vet immediately.